Reducing The Risk of Falls
Statistics on Falls
Falls have become the leading cause of injury for older adults. 27.5% of individuals 65 years and older have reported at least one fall in the past year.1 These falls can lead to serious injuries that involve broken bones or head trauma. Each year over 800,000 people in this age group are hospitalized due to a fall injury and 95% of hip fractures are caused by a fall.2 However, falls are preventable. Working to recognize the modifiable risk factors in our lives can help reduce the chance of fall and injury.
What Factors Influence falls?
Some major risk factors that contribute to increased fall risk are listed below. Falls are more likely to occur when there is a combination of these factors:3
Advancing age
Weakness
Environmental factors such as obstacles, slippery surfaces, or poor lighting
History of falling
Most of these risk factors can be managed by a medical provider such as your primary care physician and your physical therapist.Physical therapy can work to help address these risk factors such as weakness, balance, and changing your environment so that you can save a trip to the hospital. When asked about the factors contributing to a fall Dr. Gary Chimes, MD in Bellevue added, “When I see a patient who has recently fallen, my mind first goes to the question "why did they fall?" I want to distinguish between factors extrinsic to the patient (e.g., icy ground), and factors intrinsic to the patient (e.g., situational awareness, single leg balance).”
“In the acute phase after I fall, I want to assess for injuries sustained during the fall. After recovery from the injury, my intermediate and long term goals are to “rehabilitate beyond the resolution of symptoms” and address factors that can both limit the chance of another fall, and mitigate long term injury in the event that they do have a fall.”
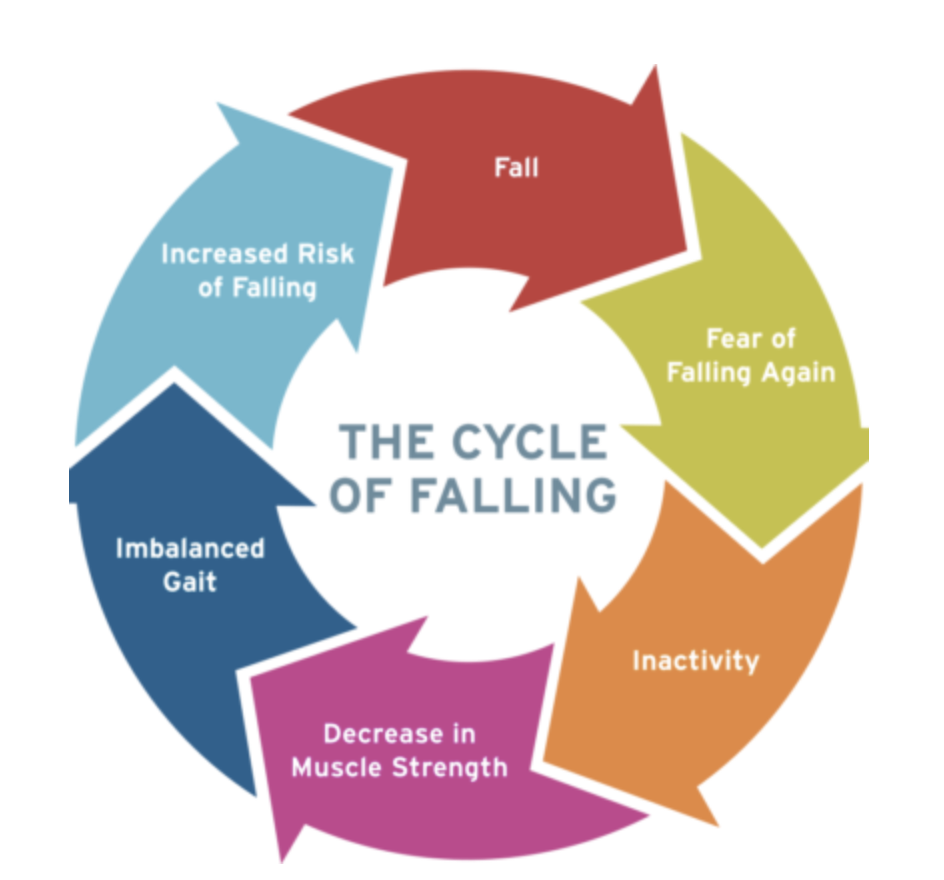
The “Fall Cycle”
As noted above, those who have a history of falls are at higher risk for additional falls. This pattern is known as the “fall cycle”.5 Individuals who have experienced a fall may develop a fear of falling due to a lack of confidence in their ability to independently navigate their home or perform daily functional activities. This fear of falling leads to a lower activity baseline, as the individual becomes less likely to participate in their usual activities throughout the day. The increase in sedentary lifestyle leads to a gradual overall loss of strength and balance, which perpetuates the likelihood of falls in the future.
“Clinicians can decrease the risk of falls in patients by improving muscle weakness and balance with physical therapy. It is also important to further evaluate medications for possible side effects/monitoring blood pressure and to assist with visual or cognitive impairments. Evaluation of the patient’s home environment is important to assess for potential fall hazards. ”
What can you do to limit the chance of falling?
Change your home environment: Make your home safer by reducing trip hazards. Clearing out cluttered walkways by removing loose wires, boxes, or taping down rugs will help decrease the chance of slipping or tripping. Consider using night lights to brighten up dark hallways or rooms to increase visibility and reduce the chance of falling. Speak to your PT for other tips and recommendations that can help decrease the risk of tripping and falling.
Routine check ups with your healthcare team: Maintain active communication with your primary care physician or pharmacist to help review medications that can induce dizziness, faintness, or drowsiness. Annual eye exams with your optometrist help ensure your visual acuity stays sharp so that you are able to recognize potential tripping hazards. Go see your local physical therapist to get assessed for fall risk. A physical therapist can work with you to address any strength and balance deficits that may be hindering your ability to safely navigate around your home and community.
Exercise and strength training: As we get older, we tend to lose muscle mass and strength at a faster rate.6 A higher percentage of older adults who reported no physical activity within the last month or adults who report difficulty with daily functional activities have reported of falls or fall related injuries.1 Incorporating a daily exercise routine can help improve mobility and balance. A physical therapist can assess your current baseline and develop an exercise routine with you to improve strength and balance.
Exercise options at home
Practice balance activities throughout the day! It doesn’t take any extra time to perform these exercises. For example, you can practice standing on one leg while brushing your teeth. Stand for 30 seconds at a time; by the time you are done brushing your teeth, you should be able to complete two sets on each leg. Single leg standing too hard? Try placing one foot in front of the other in “tandem stance” for a more moderate challenge instead.
Attend group exercise classes: Many local gyms offer free membership for adults 65 years or older through the Silver Sneakers Program. They may also offer live online classes and workshops that you can perform from the comfort of your own home. See the Silver Sneakers program for more information.
Practice getting on / off the ground: There are times when falls are inevitable. By practicing the activity of getting on and off the ground as part of your exercise routine, you will have the knowledge and capability to safely get back up if it does happen. This can be most easily accomplished by breaking down an activity into smaller tasks and learning the action in reverse order, a process known as back chaining. By starting in the most stable position of the process (sitting in a chair), you allow yourself to begin in a safe environment and progress towards stages that are more unstable (such as kneeling or laying down). You can work with your physical therapist to help build your confidence and strength so that you can safely get on and off the ground. Remember that in the event that you do happen to fall, a few steps may be necessary steps prior to getting up:
Stay calm
Check if the environment is safe to move around in
Access the injury and determine if you are safe and able to move
Call for help if needed
If you think you can get up but require assistance, move to a chair or other sturdy object you can hold onto to help pull yourself up
Follow up with a primary care doctor or physical therapist to determine any significant injuries
What can physical therapy do for you?
Fear of falling can lead to social withdrawal and inactivity, and ultimately to decreased independence in your daily life. When asked about this Dr. Irene Young, MD in Bellevue commented, “Physical therapists play a critical role as they work with patients on a more frequent basis and can oversee their balance and strengthening program. Finding out about the patients day to day activities and potential fall hazards are important. Patients may also need to consider assistive devices at home and in the community to help with balance and gait.”
Physical therapy can help you break the Fall Cycle and regain your independence by working to improve your strength and balance. Starting a home exercise program under supervision of a PT is a proactive way to stay safe and reduce your fall risk. Stop in and see your physical therapist today!
AUTHOR:
Hork Do, PT, DPT
LWPT Redmond Physical Therapist
CONTRIBUTORS:
Dr. Gary Chimes, MD
Lake Washington Sport & Spine Physiatrist
Dr. Irene Young, MD
Swedish Physical Medicine & Rehabilitation
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
Founder & Director Lake Washington Physical Therapy
References
Moreland B, Kakara R, Henry A. Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years - United States, 2012-2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):875-881. Published 2020 Jul 10. doi:10.15585/mmwr.mm6927a5
Parkkari J, Kannus P, Palvanen M, Natri A, Vainio J, Aho H, Vuori I, Järvinen M. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int, 1999;65:183–7.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013 May;75(1):51-61. doi: 10.1016/j.maturitas.2013.02.009. Epub 2013 Mar 22. PMID: 23523272.
Facts about falls. Centers for Disease Control and Prevention. https://www.cdc.gov/falls/facts.html. Published August 6, 2021. Accessed January 5, 2022.
Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997 May;26(3):189-93. doi: 10.1093/ageing/26.3.189. PMID: 9223714.
Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2014;3(4):346-350. Published 2014 Feb 24.