What is the SC Joint?
Sternoclavicular Joint Reconstruction:
Contemporary Stabilization Procedures and Rehabilitative Care with Case Report
Sternoclavicular Joint Background:
Acute and chronic sternoclavicular (SC) dislocations are rare. Due to the rarity, consistent assessment and treatment experience among medical providers is lacking. Recognizing the type and extent of injury to the SC joint requires a high index of suspicion, a comprehensive evaluation, and proper imaging studies. Many disorders of the SC joint can be treated non-operatively. However, surgical treatment may be indicated for irreducible dislocations and symptomatic, chronic instability that fails non-operative physical therapy. The purpose of this paper is to provide a comprehensive update on the current surgical techniques supported by anatomic, biomechanical, and outcome data that a rehabilitation specialist can expect to encounter.
Case Description:
This case details the physician assessment, surgical procedure, physical therapy treatment, and outcome of an active, 15 year-old male with atraumatic SC joint instability. A criterion-based rehabilitation guideline, in conjunction with the author’s clinical decision making, manual therapy intervention, and an understanding of the surgical technique, served as the framework for the patient’s post-operative progression. The patient returned to full-participation in sports at 7 months and he remained symptom free without functional limitations at 1 year following surgery.
Discussion:
The rarity of SC joint instability may create a gap in a physical therapists ability to recognize, treat, and post-operatively manage these patients successfully. The figure-of-8 graft reconstruction technique may be recommended more frequently due to recent favorable biomechanical and outcome research. Additional biomechanical research and stratified outcome studies will be needed to better understand adaptations in the shoulder girdle that a physical therapist may expect to find when working with these patients.
“Elevation and depression occur between the clavicle and SC disk, whereas protraction and retraction occur between the disk and the manubrium. The ligaments that stabilize the SC joint are essential for its 50° of clavicular rotation, 35° of elevation, and 35° of anterior-posterior glide.”
SC Joint Dislocations:
Sternoclavicular joint dislocations are rare injuries, representing only 2-3% of the injuries of the upper limb.1 Although rare, such injuries deserve rapid diagnosis and effective treatment to avoid future complications. Motor vehicle collisions and sports participation are the top two causes of traumatic SC joint injury.2,3,4 The injury can be classified on the basis of anatomy in posterior or anterior dislocation, etiology into direct trauma, indirect trauma, or atraumatic injuries, and to the degree of ligamentous injury.2,5 In 1967, Allman classified SC joint injuries based on the degree of ligamentous disruption. Type 1 describes a simple sprain of the SC ligaments and capsule without subluxation or dislocation. Type 2 injuries involve a disruption of the SC ligaments and capsule and result in a subluxation of the medial clavicle without dislocation. Type 3 injuries entail a rupture of all supporting ligaments with complete anterior or posterior dislocation.6
Anatomy and Biomechanics of the SC Joint
The development of the clavicle is unique compared to other bones in the body. Although it is the first long bone to ossify in the womb during the fifth gestational week, its physis is the last to close at nearly 25 years of age. As such, many SC joint dislocations in younger patients may be the result of injury to a non united epiphysis rather than ligamentous disruption.7,8,9
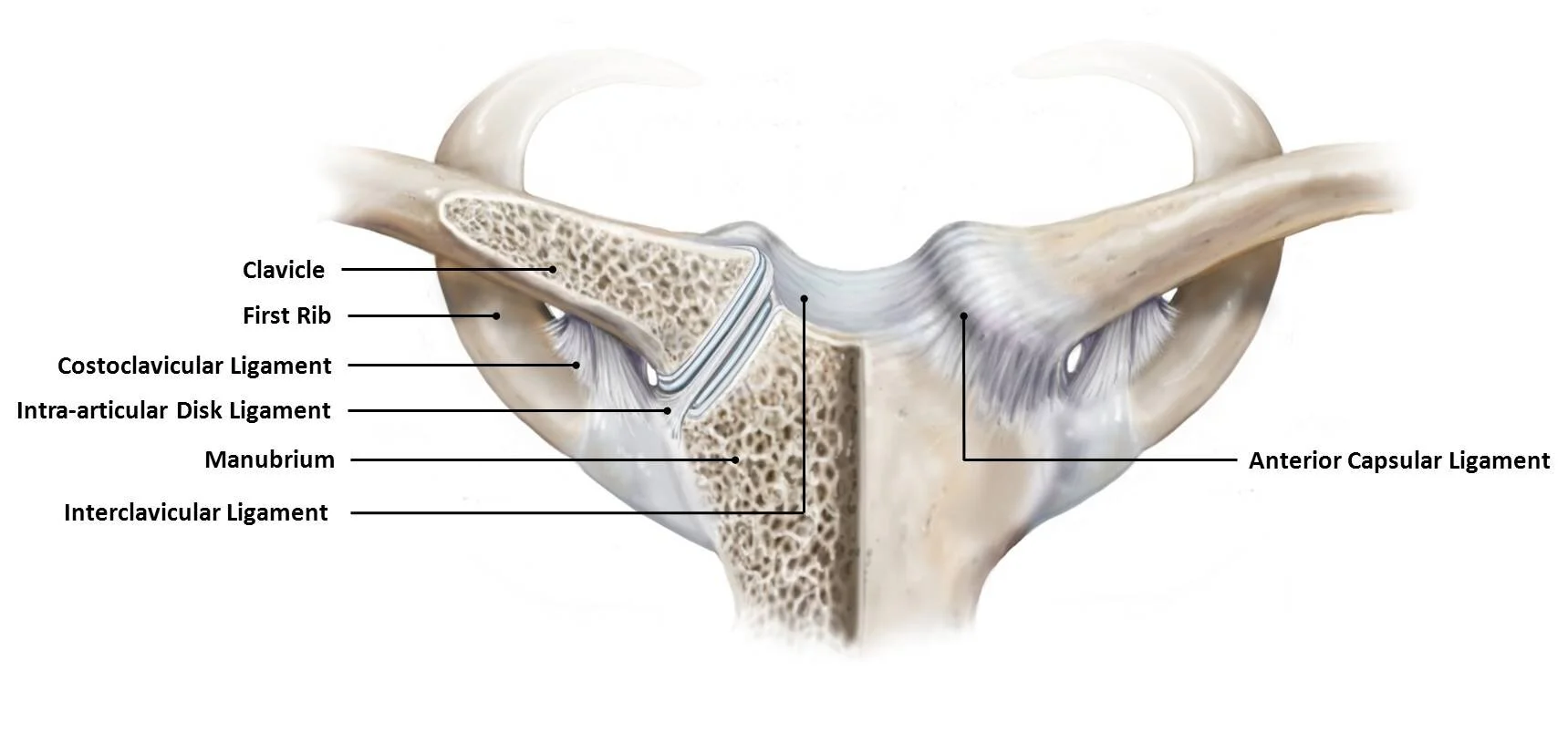
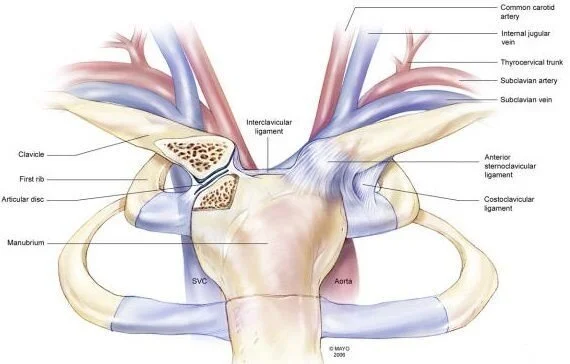
Figure 1. Osseoligamentous anatomy of the sternoclavicular joint.
The SC joint is an incongruous, diathrodial saddle joint composed of the medial clavicle, sternum, and first rib.10 The surfaces of the SC joint are covered with fibrocartilage and are highly incongruent. Osseous stability of the SC joint is among the lowest of the major joints in the body because less than half of the medial clavicle articulates with the superior angle of the sternum.11 As a result, this incongruity requires stability from its surrounding ligamentous supports. The SC joint articulation is held in place by the SC capsular ligaments, the costoclavicular ligament, and the interclavicular ligament (Figure 1). A fibrocartilaginous disc acts primarily as a restraint against medial displacement of the proximal clavicle and blends with the fibers of the capsular ligament anteriorly and posteriorly.10
The anatomy of the joint surfaces and ligaments dictates the functional movement at the SC joint. The arthrokinematic motion is similar whether the shoulder girdle moves actively or passively. During scapular elevation, the medial clavicle glides inferiorly on the sternum. Depression of the scapula elicits a superior glide of the medial clavicle on the sternum. The medial clavicle moves posteriorly with scapular protraction and anteriorly with scapular retraction. When the clavicle moves in one direction, the capsular ligaments on the side of the motion become lax. Ligaments on the opposite side of the joint become taut, limiting the movement.12 The axis of motion lies lateral to the joint at the costoclavicular ligament. The location of the axis so far from the joint accentuates the intra-articular motion with elevation-depression and protraction-retraction.13
Elevation and depression occur between the clavicle and SC disk, whereas protraction and retraction occur between the disk and the manubrium.14 The ligaments that stabilize the SC joint are essential for its 50° of clavicular rotation, 35° of elevation, and 35° of anterior-posterior glide. The anterosuperior and posterior aspects of the capsular ligament provide the primary support for the SC joint, with greater strength provided by the posterior component. In 1967, Bearn demonstrated that the capsular ligament is the most important structure preventing superior displacement of the medial clavicle and inferior descent of the distal clavicle.15 More recently Spencer et al. performed a cadaveric biomechanical study to demonstrate that the posterior SC joint capsule is the most important structure for preventing both anterior and posterior translation of the SC joint, with the anterior capsule acting as an important secondary stabilizer.16 Dennis et al. also found that it took 50% more force to dislocate the clavicle posteriorly, compared to anteriorly, in cadavers.17
Mechanism of Injury
Anterior dislocation is three to twenty times more common than posterior dislocation.2,18 Posterior dislocation, which is rare, may cause serious complications due to compression of prime central structures by the medial clavicle (Figure 2). Respiratory discomfort, lesions of the brachial plexus, and arterial insufficiency are some of the harmful consequences of this type of dislocation.19,20,21,22 The high rate of complications and their severity emphasize the importance of an accurate diagnosis and treatment plan.
Some of the factors contributing to SC joint stability include the particular collagen makeup of the patient’s ligaments, the arrangement of the SC ligaments and their method of attachment, and the variation in osseous anatomy of this saddle type joint. This small, incongruous joint is subject to practically every motion of the upper extremity, however the ligamentous support and design make it one of the least dislocated in the body.10
The direction of direct force to the clavicle often determines the type of dislocation.
When a force is applied directly to the anteromedial aspect of the clavicle, the clavicle is pushed posteriorly behind the sternum and into the mediastinum. This may occur in a variety of ways: for example, when an athlete is jumped on while lying on their back, the contact is directly on the medial end of the clavicle; when a kick is delivered to the front of the medial clavicle; when a person is run over by a vehicle; or when a person is pinned between a vehicle and a wall or the ground.
An indirect force can be applied to the SC joint from either the anterolateral or posterolateral aspect of the shoulder. If the shoulder is compressed and rolled backward, the anterolateral applied force produces an anterior dislocation of the SC joint as the underlying first rib acts as a fulcrum to lever the sternal end of the clavicle anteriorly.10 By contrast, a posterolateral compression on the shoulder moves it forward and the force directed toward the clavicle produces a posterior dislocation.23
Spontaneous atraumatic anterior subluxation of the SC joint is less likely to occur compared to indirect or direct trauma of the clavicle. When it does occur, it is most commonly seen in teenagers and young adults who have ligamentous laxity. The subluxation often occurs either during routine overhead activities or during overhead sports activities.5
More Shoulder Articles & FAQs
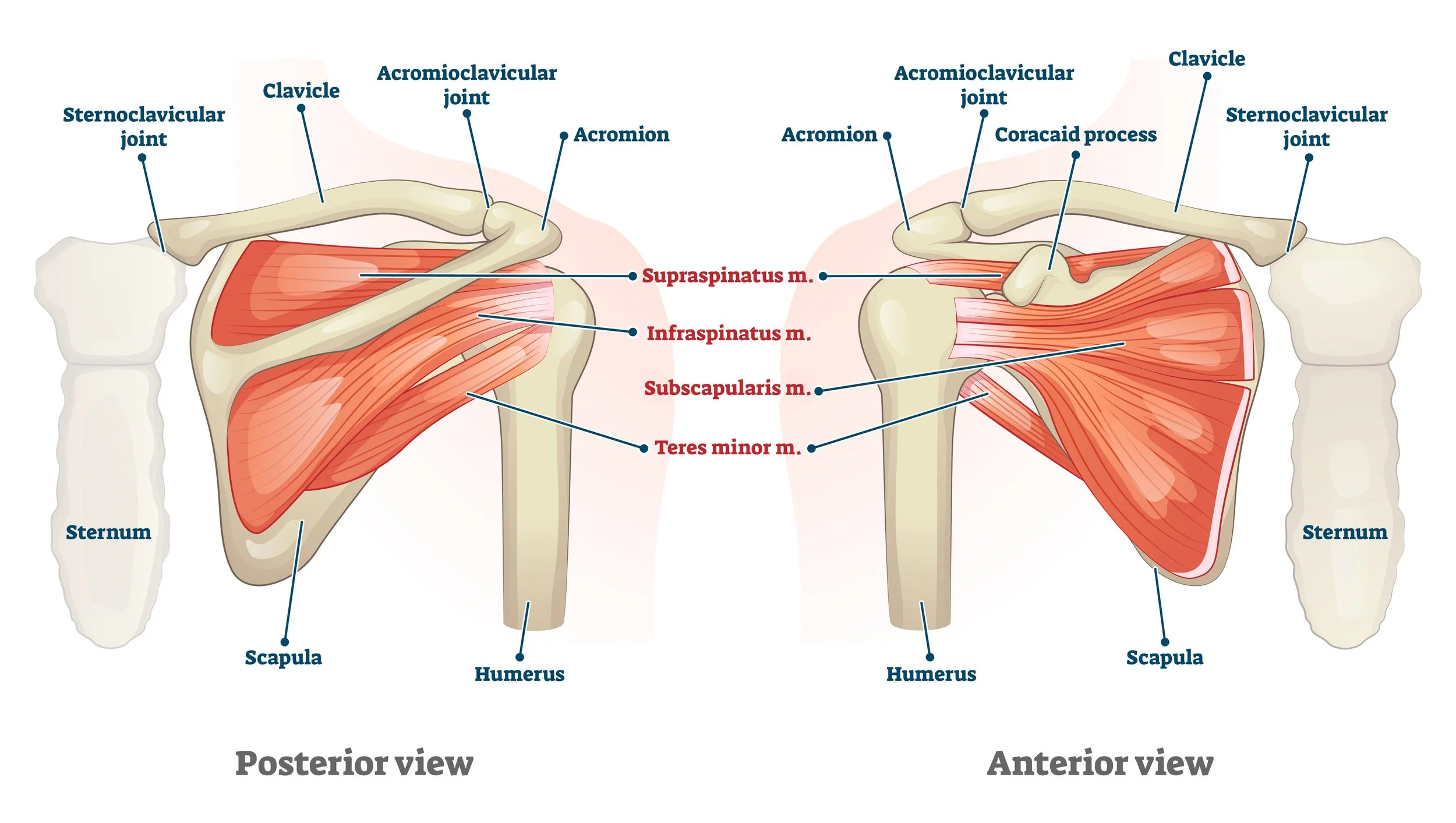
What Exercises Are Bad for the Rotator Cuff?
How Can I tell If I Have a Strain or Torn Rotator Cuff?
What Are the Tests for a Rotator Cuff Tear?
Do I need an MRI or MRI Arthrogram for my Shoulder?
What is Wrong With My Shoulder?
What is Rotator Cuff Tendinitis?
Contributing Authors, Collaborators, & Colleagues:
Mark Bouma, PT, DPT, OCS,COMT,FAAOMPT,CSCS
Heidi Biehl, PT, DPT, OCS, CSCS, CFSC
Matt Sato, PT, TPIc, SFMA
Benjamin Wobker, PT, MSPT, CSCS, SFMA
Joe nance, PT, MPT, OCS, COMT, FAAOMPT, ATC
DR. Samuel Koo, MD
DR. Jamie Antoine, MD
Dr. Vincent Santoro, MD
Dr. Camile Clinton, MD
Dr. Bob AdamS, DO
Dr. Christian Peterson, DO
DR. Chris Wahl, MD
Dr. Dayne Mickelson, MD
DR. Tyler Nathe, MD
Dr. Thomas CastLe,MD
Dr. Michael Sailer, MD
Dr. Greg Komenda, MD
References:
1 Groh GI, Wirth MA. Management of traumatic sternoclavicular joint injuries. J Am Acad Orthop Surg. 2011; 19: 1-7.
2 Nettles JL, Linscheid RL. Sternoclavicular dislocations. J Trauma. 1968; 8:158-64. 3 Waskowitz W. Disruption of the sternoclavicular joint: analysis and review. Am J Orthop. 1961;3:176-9.
4 Omer GE Jr. Osteotomy of the clavicle in surgical reduction of anterior sternoclavicular dislocation. J Trauma. 1967;7:584-90.
5 Rockwood CA, Odor JM. Spontaneous atraumatic anterior subluxation of the sternoclavicular joint. J Bone Joint Surg Am. 1989;71:1280-8.
6 Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49(4):774-784.
7 El Mekkaoui MJ, Sekach N, BazeilA, Faustin JM. Proximal clavicle physeal fracture separation mimicking an anterior sternoclavicular dislocation. Orthop Traumatol Surg Res. 2011;97(3):349-352.
8 Koch MJ, Wells L. Proximal clavicle physeal fracture with posterior displacement: diagnosis, treatment, and prevention. Orthopedics. 2012;35(1):e108-111. 9 Webb PA, Schuey JM. Epiphyseal union of the anterior iliac crest and medial clavicle in a modern multiracial sample of American males and females. Am J Phys Anthropol. 1985;68:457-466.
10 Wirth MA, Rockwood Jr C. Disorders of the sternoclavicular joint: pathophysiology, diagnosis, and management. Philadelphia: Lippincott Williams & Wilkins; 1999. P. 765-813.
11 Flatow EL. The biomechanics of the acromioclavicular, sternoclavicular, and scapulothoracic joints. In: Heckman JD, editor. Am Acad of Ortho Surg. 1993. P. 237-45.
12 Peat M. Functional anatomy of the shoulder complex. Phys Ther. 1986;66:1855- 1865.
13 Norkin CC, Levangie PK. Joint structure and function: a comprehensive analysis. 2nd edition. Philadelphia: F.A. Davis; 1992. P 211-214.
14 Zuckerman JD, Matsen III FA. Biomechanics of the shoulder. In: Nordin M, Frankel VH, editors. Basic biomechanics of the musculoskeletal system. 2nd edition. Philadelphia: Lea & Febiger; 1989. P. 225-47.
15 Bearn JG. Direct observations on the function of the capsule of the sternoclavicular joint in the clavicular support. Anat. 1967; 101:159-70. 16 Spencer EE, Kuhn JE, Huston LJ, Carpenter JE, Hughes RE. Ligamentous restraints to anterior and posterior translation of the sternoclavicular joint. J Shoulder Elbow Surg. 2002;11:43-7.
17 Dennis MG, Kummer FJ, Zuckerman JD. Dislocations of the sternoclavicular joint. Bull Hosp Jt Dis. 2000;59(3):153-7.
18 Rockwood CA Jr, Green DP, Bucholz RW. 1991. Fractures in adults. JB Lippincott, Philadelphia, 1253-1307.
19 Borrero E. Traumatic posterior displacement of the left clavicular head causing chronic extrinsic compression of the sub avian artery. Phys Sportsmed. 1987;15:87- 89.
20 Gangahar DM, Flogaites T. 1978. Retrosternal dislocation of the clavicle producing thoracic outlet syndrome. J Trauma. 18: 369-372.
21 Homdahl HC. 1953. A case of posterior sternoclavicular dislocation. Act Orthop Scand. 23:218-222.
22 Louw JA, Louw JA. 1987. Posterior dislocation of the sternoclavicular joint associated with major spinal injury: a case report. S Afr Med J. 71: 791-792. 23 MacDonald PB, Lapointe P. Acromioclavicular and sternoclavicular joint injuries. Orthop Clin North Am. 2008;39:535-45.
24 Habernek H, Hertz H. Origin, diagnosis and treatment of sternoclavicular joint dislocation. Aktuelle Traumatol. 1987;17:23-8.
25 Hobbs DW. Sternoclavicular joint: A new axial radiographic view. Radiology. 1968;90:801.
26 Wirth MA, Rockwood CA. Disorders of the sternoclavicular joint. In: The Shoulder. 4th ed. Rockwood CA Jr, Matsen FA III, Wirth MA, Lippitt SB, eds. Philadelphia, PA: Saunders; 2009:527-560.
27 Wirth MA, Rockwood CA. Acute and chronic traumatic injuries of the sternoclavicular joint. J Am Acad Orthop Surg. 1996;4:268-78.
28 Iannotti JP, Williams GR. Disorders of the Shoulder: Diagnosis and Management. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:765-813. 29 Van Holsbeeck M, van Melkebeke J, Dequeker J, Pennes DR. Radiographic findings of spontaneous subluxations of the sternoclavicular joint. Clin Rheumatol. 1992;11(3):376-381.
30 Chaudhry FA, Killampalli VV, Chowdhry M, Holland P, Knebel RW. Posterior dislocation of the sternoclavicular joint in a young rugby player. Acta Orthop Traumatol Turc. 2001;45(5):376-378.
31 Bicos J, Nicholson GP. Treatment and results of sternoclavicular joint injuries. Clin Sports Med. 2003;22(2):359-70.
32 Iannotii J, Williams Jr G. Disorders of the shoulder: diagnosis and management. 2nd edition. Philadephia: Lippincott Williams & Wilkins; 2007. P. 979-1006. 33 Thomas DP, Davies A, Hoddinott HC. Posterior sternoclavicular dislocations—a diagnosis easily missed. Ann R Coll Surg Engl. 1999 May;81(3):201-4. 34 Lunseth PA, Chapman KW, Frankel VH. Surgical treatment of chronic dislocations of the sterno-clavicular joint. J Bone Joint Surg Br. 1975;57(2):193-196. 35 Yeh GL, Williams GR Jr. Conservative management of sternoclavicular injuries. Orthop Clin North Am. 2000;31(2):189-203.
36 Van Tongel A, McRae S, Gilhen A, Leiter J, MacDonald P. Management of anterior sternoclavicular dislocation: a survey of orthopedic surgeons. Acta Orthop Belg. 2012;78(2):164-169.
37 Robinson CM, Jenkins PF, Markham PE, et al. Disorders of the sternoclavicular joint. J Bone Joint Surg Br. 2008 Jun;90(6):685-96.
38 Thut D, Hergan D, Dukas A, Day M, Sherman OH. Sternoclavicular joint reconstruction: a systematic review. Bull NYU Hosp Jt Dis. 2011;69(2):128-35. 39 Ferrandez L, Yubero J, Usabiaga J, et al. Sternoclavicular dislocation. Treatment and complications. Ital J Orthop Traumatol. 1988 Sep;14(3):349-55. 40 Franck WM, Jannasch O, and Siassi M, et al. Balser plate stabilization: an alternate therapy for traumatic sternoclavicular instability. J Shoulder Elbow Surg. 2003 May;12(3):276-81.
41 Rockwood CA, Groh GI, Wirth MA, et al. Resection arthoplasty of the sternoclavicular joint. J Bone Joint Surg Am. 1997 Mar;79(3)387-93. 42 Bae DS, Kocher MS, Waters PM, et al. Chronic recurrent anterior sternoclavicular joint instability: results of surgical management. J Pediatr Orthop. 2006 Jan;26(1):71-4.
43 Abiddin Z, Sinopidis C, Grocock CJ, et al. Suture anchors for treatment of sternoclavicular joint instability. J Shoulder Elbow Surg. 2006 May-Jun;15(3):315-8. 44 Armstrong AL, Dias JJ. Reconstruction for instability of the sternoclavicular joint using the tendon of the sternocleidomastoid muscle. J Bone Joint Surg Br. 2008 May;90(5):610-3.
45 Thomas DP, Williams PR, Hoddinott HC. A ‘safe’ surgical technique for stabilization of the sternoclavicular joint: a cadaveric and clinical study. Ann R Coll Surg Engl. 2000 Nov;82(6):432-5.
46 Spencer EE, Kuhn JE. Biomechanical analysis of reconstructions for sternoclavicular joint instability. J Bone Joint Surg Am. 2004 Jan;86(1):98-105. 47 Martetschlager F, Warth RJ, Millett PJ. A current concepts review: instability and degenerative arthritis of the sternoclavicular joint. Am J Sports Med. 2013;20(10):1- 9.
48 Castrophil W, Ramadan LB, Bitar AC, Schor B, de Oliveira D’Elia C. Sternoclavicular dislocation—reconstruction with semitendinosus tendon allograft: a case report. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):865-868.
49 Friedrich L, Afifi FK, Skarvan J, Friedrich NF, Hirschmann MT. Combined gracilis tendon autograft reconstruction and discus repair of a chronic anterior-superior sternoclavicular joint dislocation. Knee Surg Sports Traumatol Arthosoc. 2012;20(1):1978-1982.
50 Guan JJ, Wolf BR. Reconstruction for anterior sternoclavicular joint dislocation and instability. J Shoulder Elbow Surg. 2013;22(6):775-781.
51 Jesacher M, Singer G, Hollwarth ME, Eberl R. Traumatic posterior dislocation of the sternoclavicular joint: a case report of joint stabilization with gracilis tendon graft. Unfallchirurg. 2012;115(2):165-168.
52 Singer G, Ferlic P, Kraus T, Eberl R. Reconstruction of the sternoclavicular joint in active patients with the figure-of-eight technique using hamstrings. J Shoulder Elbow Surg. 2013;22(1):64-69.
53 Millett PJ. Adapted from operative report. Vail Valley Medical Center. Vail, CO. 2012.
54 Schunk C and Rutt R. TAOS Functional Index: Orthopaedic rehabilitation outcomes tool. J Rehabil Outcomes Meas. 1998, 2(2), 55-61.
55 Maitland GD. Peripheral Manipulation. London: Butterworths; 1978. 56 Cyriax J and Russell G. Textbook of orthopaedic medicine—Vol II.—treatment by manipulation and injection. 10th ed. Bailliere Tindall, London. 1980, 13-22.
Disclaimer:
This website is an information and education resource for health professionals and individuals with injuries. It is not intended to be a service for patients and should not be regarded as a source of medical or diagnostic determination, or used as a substitute for professional medical instruction or advice. Not all conditions and treatment modalities are described on this website. Any liability (in negligence or otherwise) arising from any third party acting, or refraining from acting, on any information contained on this website is hereby excluded.