IT Band Syndrome
What is Illiotibial Band Syndrome?
Iliotibial band syndrome (ITBS) is a common overuse injury characterized by pain at the outside of the knee. It’s particularly prevalent in endurance athletes such as runners and cyclists-- those who undergo repetitive back-and-forth knee movements. In fact, ITBS is the leading cause of lateral knee pain and the second leading cause of overall knee pain in this population.
“Illiotibial Band Syndrome can be a very frustrating injury for even the most successful runners. I have seen this injury affect recreational runners and Olympic caliber athletes approaching international competition.”
Illiotibial Band Background
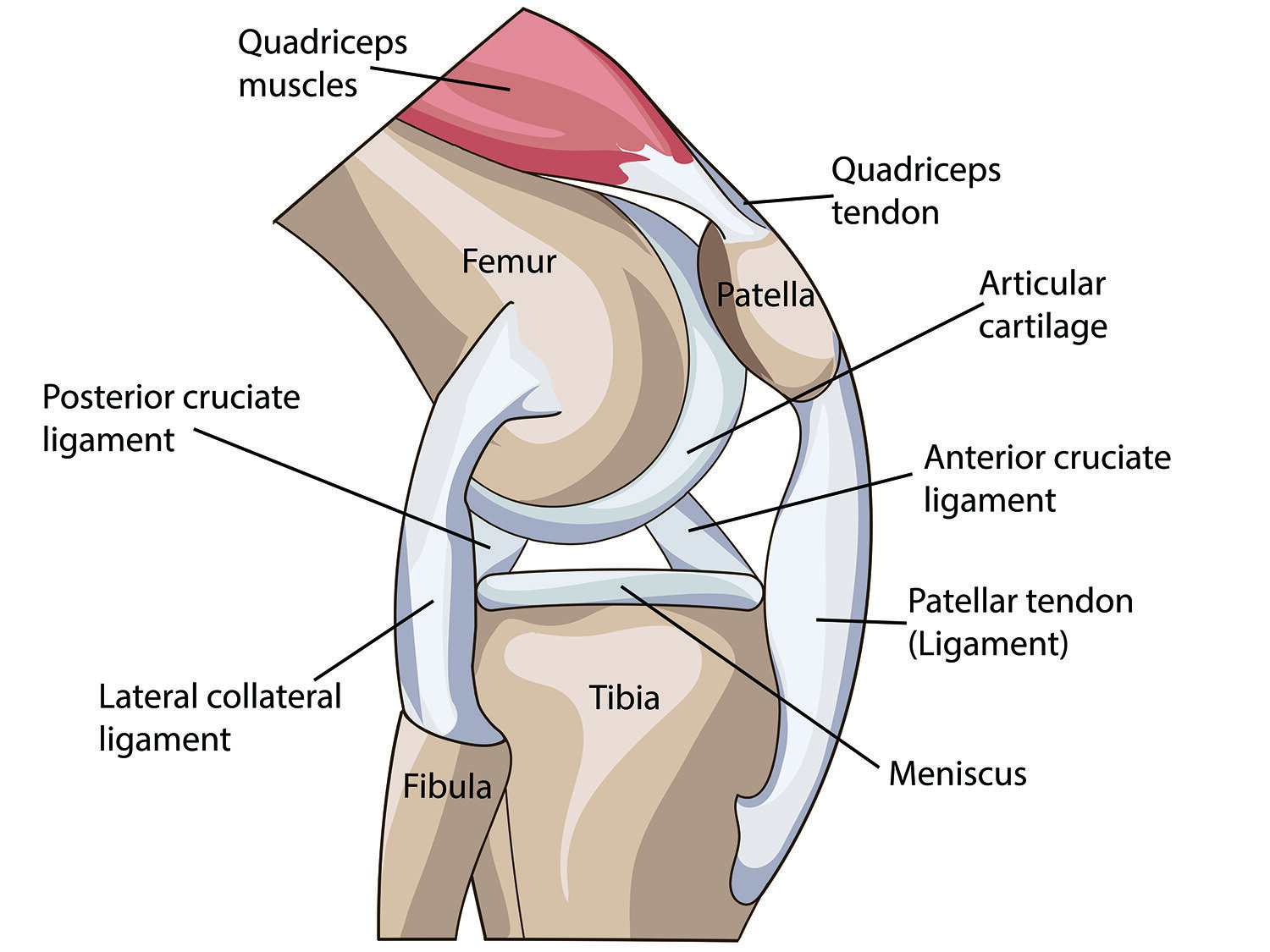
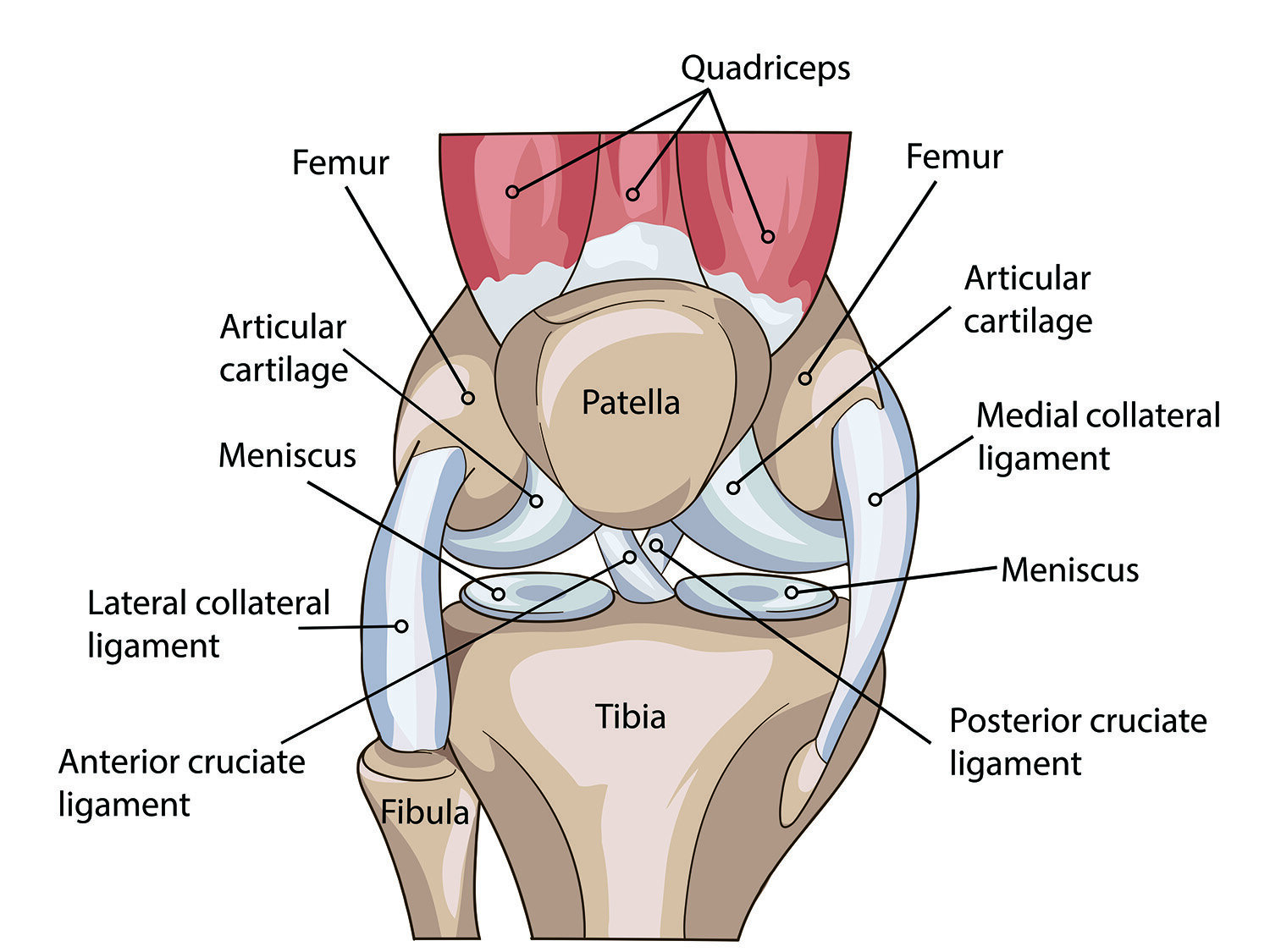
The ITB is a long, nonelastic area of fascia (connective tissue) that starts above the hip joint, extends all the way down the side of the thigh, and attaches just below the outside of the knee. Near its origin at the iliac crest (the bony ridge of your pelvis, just below your natural waist), the fibers of the ITB blend into the fibers of a muscle called the tensor fascia lata (TFL). The ITB shifts forward and backward with motion at the knee, as the fascial layer glides over the muscles in the thigh.
What Causes IT Band Syndrome?
When we asked Dr. Troy Henning, DO from Swedish Hospital his thoughts on iliotibial band syndrome he stated, “ITBs at the knee in runners can be related to poor neuromuscular control of the hip girdle and ankle stabilizers/foot intrinsics. Essentially excessive hip adduction as seen with weak hip abductor/adductor balance”. What does this mean? Runners and hikers will need to achieve more balance between strength an flexibility on the inner and outer hip. Dr. Henning adds, “core muscles can allow the pelvis to drop excessively on the swing side and lead to hip adduction on the stance leg. This then tensions the IT band from the pelvis down across the knee and may lead to rubbing at the lateral femoral condyle.
The traditional theory behind the mechanism of ITB pain focuses on the forward-backward shift of the ITB over the lateral femoral condyle, a bony prominence at the outside of your knee. When there is excessive tightness in the band, one section of the ITB rubs over the femoral condyle as the knee flexes and extends, resulting in pain at the outside of the knee. However, a secondary theory posits that the pain is actually from compression of a small fat pad underneath the ITB at the lateral knee, not from the band itself. This fat pad becomes compressed with movements that tension the band-- for example, when you bend your knee or rotate the leg inward.
When we asked Evergreen Orthopedics & Sports Medicine surgeon Dr. Camille Clinton, MD she added, “I see ITBs most frequently in runners. The most common underlying causes are tightness (esp ITB tightness), lack of hip/glut strength, poor running form and alignment/pronation/improper or not ideal shoes.”
“I like to do a OBER test and plan my treatment accordingly. When the OBER is negative, the cause is most likely to be weakness (glutes and Core) and issue with alignment/leg lenght and/or technique. When the OBER is positive (tight ITB) , Foam rolling , deep soft tissue massage and dry needling (TFL) are important to add , in addition to the above”
Dr. Troy Henning, DO from Swedish Hospital supported similar thoughts. He states that, “ITBS at the knee in runners can be related to poor neuromuscular control of the hip girdle and ankle stabilizers/foot intrinsics-- essentially excessive hip adduction, as seen with weak hip abductor/adductor balance”. What does this mean? Runners and hikers will need to achieve more balance between strength and flexibility on the inner and outer hip. Dr. Henning adds, “[Weakness in] core muscles can allow the pelvis to drop excessively on the swing side, and lead to hip adduction on the stance leg. This then tensions the IT band from the pelvis down across the knee and may lead to rubbing at the lateral femoral condyle.
What about the foot and ankle, you might ask? Dr. Henning states that, “If the foot is going into excessive pronation because of relatively weak tibialis posterior/foot intrinsics or tight triceps surae, the tibia may internally rotate more than what is ideal. As the ITB inserts on the Gerdy's tubercle of the tibia, the excessive internal rotation of the tibia will cause tensioning of the ITB and again can lead to excessive friction along the lateral femoral condyle and/or synovial tissue. Additionally, intrinsic knee pathology that leads to a chronic effusion may tension the IT band and lead to rubbing [as well].”
Other factors that can increase your risk of ITBS include:
Training errors: A sudden change in frequency or intensity of activity can result in an overuse injury. In the case of ITBS, repetitive movements through knee flexion and extension put stress on the involved structures. Although these movements are a component of normal daily life, overuse injuries occur when the amount of load through the joint exceeds the tissue’s ability to recover on a timely basis.
Anatomical factors: The geometry of your body affects the distribution of load through specific structures. Individuals with differences in limb length, an abnormal knee angle (either “knock kneed” or “bow legged”), excessive foot pronation (inward collapse of the midfoot), weak hip musculature, or an excessively tight ITB may be more prone to this injury.
Biomechanical factors: Structural differences aside, the way your body moves may also affect the distribution of load through the ITB and nearby tissues. This includes muscle weakness or relative imbalance among the quadriceps, hamstrings, or gluteus muscles. Additionally, poor motor control may result in increased landing forces in each step or cycle of sport-specific movements. Any one of these may contribute to the development of ITBS.
We asked longtime colleague and prominent physiatrist at Swedish, Dr. Irene Young her thoughts what she sees in her practice. Dr. Young is a runner herself as well as her husband. She states, “Common causes of ITBS in our patients include muscle imbalances, anatomical variation and training habits.”
“ITBS can be frustrating to treat for some athletes as it can take a considerable amount of time and rehabilitation to treat the condition. Mainstay treatments often involve relative rest, NSAIDs, physical therapy, possible injections or for more intractable cases surgery”
Iliotibial Band Treatments
Gait and movement retraining to improve the dynamic alignment of your knees, so that you can better perform activities including walking, running, jumping, squatting, and other sport-specific movements
Strength training targeting gluteus muscles and other key groups for knee stabilization, including your quadriceps, hamstrings, hip rotator muscles, and core
Stretching and soft tissue mobilization to increase flexibility of your iliotibial (IT) band, lateral fascia, TFL, quadriceps, hamstrings, and calf
Manual therapy and taping to directly address knee biomechanics
Footwear and orthoses to support improved alignment of your knees and lower extremities during daily activities and sport-related movement
Education about proper running form and training progression
Ice, active recovery, and appropriate rest to reduce pain and inflammation at the knee joint
Dr. Irene Young adds in terms of treatment, “We recommend a conservative approach to treating ITBS including physical therapy and most will recover. If a patient fails to improve after conservative treatments than we will consider procedures such as cortisone injections or PRP/stem cell.”
“A runner or hiker should not have to be plagued by ITBs their entire life.”
Dr. Henning adds, “Most of the biomechanical challenges can be corrected through proper education, development and maintenance of a strengthening/neuromuscular control and flexibility program targeting the imbalances. If appropriate shoe inserts can lead to correction of the improper foot biomechanics and resolution or control of the IT band syndrome. Once the individualized plan is established it should be maintained for the duration of their running/hiking career to prevent the problem from resurfacing. In short, no, a runner or hiker should not have to be plagued by ITBs their entire life.”
Common IT Band Symptoms
The most common symptom of ITBS is a dull, achy pain at the outside of your knee. This may be aggravated by running, jumping, cycling, or squatting, and is usually relieved with rest. Other common symptoms include:
Swelling
Popping or crackling sensations
Stiffness
Weakness
How Can Physical Therapy Help IT Band Syndrome?
Physical therapy can get you back on your feet and on the road to recovery, even with chronic or severe knee pain. Due to the many root causes of ITBS, treatment is unique to the individual. Dr. Clinton adds about ITB patients, “Most frustrating thing about ITBs for patients is often if hurts enough that you can't run or train through it. Also it can take a while to get better and often occurs when people are increasing mileage or getting back into running so it’s frustrating to have to slow down, cross train, rehab, and rest. The most frustrating thing from my standpoint is I don't have a simple "quick fix" for clients.
AUTHOR:
CONTRIBUTORS:
Dr. Bob Adams, DO, Frm USA Track & Field Head Medical Physician
Dr. Camille Clinton, MD
Dr. Troy Henning, DO
Dr. Ghislaine Robert, MD, Frm Canadian Track & Field Team Physician
Dr. Christopher Wahl, MD
Dr. Irene Young, MD
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
More Related Articles
References
Iliotibial Band Friction Syndrome. OrthoInfo: American Academy of Orthopedic Surgeons. 2020. Web. https://www.orthobullets.com/knee-and-sports/3019/iliotibial-band-friction-syndrome
van der Worp MP, et al. Iliotibial band syndrome in runners: a systematic review. Sports Med. 2012 Nov 1;42(11):969-92. doi: https://doi.org/10.1007/BF03262306.
Strauss EJ, et al. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011 Dec;19(12):728-36. doi:10.5435/00124635-201112000-00003. https://pubmed.ncbi.nlm.nih.gov/22134205/
WILLSON JD, RATCLIFF OM, MEARDON SA, WILLY RW. INFLUENCE OF STEP LENGTH AND LANDING PATTERN ON PATELLOFEMORAL JOINT KINETICS DURING RUNNING. SCAND J MED SCI SPORTS. 2015 DEC;25(6):736-43. DOI: 10.1111/SMS.12383. EPUB 2015 JAN 14. PMID:255855895.
ALLEN DJ. TREATMENT OF DISTAL ILIOTIBIAL BAND SYNDROME IN A LONG DISTANCE RUNNER WITH GAIT RE-TRAINING EMPHASIZING STEP RATE MANIPULATION. INT J SPORTS PHYS THER. 2014 APR;9(2):222-31. PMID:24790783
LENHART RL, THELEN DG, WILLE CM, CHUMANOV ES, HEIDERSCHEIT BC. INCREASING RUNNING STEP RATE REDUCES PATELLOFEMORAL JOINT FORCES. MED SCI SPORTS EXERC. 2014 MAR;46(3):557-64. DOI: 10.1249/MSS.0B013E3182A78C3A. PMID: 23917470
MEARDON SA, CAMPBELL S, DERRICK TR. STEP WIDTH ALTERS ILIOTIBIAL BAND STRAIN DURING RUNNING. SPORTS BIOMECH. 2012 NOV;11(4):464-72. PMID: 23259236
HOBARA H, SATO T, SAKAGUCHI M, SATO T, NAKAZAWA K. STEP FREQUENCY AND LOWER EXTREMITY LOADING DURING RUNNING. INT J SPORTS MED. 2012 APR;33(4):310-3. DOI: 10.1055/S-0031-1291232. EPUB 2012 MAR 1. PMID: 22383130
SCHUBERT AG, KEMPF J, HEIDERSCHEIT BC. INFLUENCE OF STRIDE FREQUENCY AND LENGTH ON RUNNING MECHANICS: A SYSTEMATIC REVIEW. SPORTS HEALTH. 2014 MAY;6(3):210-7. DOI: 10.1177/1941738113508544. PMID:24790690
LENHART R, THELEN D, HEIDERSCHEIT B. HIP MUSCLE LOADS DURING RUNNING AT VARIOUS STEP RATES. J ORTHOP SPORTS PHYS THER. 2014 OCT;44(10):766-74, A1-4. DOI: 10.2519/JOSPT.2014.5575. EPUB 2014 AUG 25.PMID: 2515604
CHUMANOV ES, WILLE CM, MICHALSKI MP, HEIDERSCHEIT BC. CHANGES IN MUSCLE ACTIVATION PATTERNS WHEN RUNNING STEP RATE IS INCREASED. GAIT POSTURE. 2012 JUN;36(2):231-5. DOI: 10.1016/J.GAITPOST.2012.02.023. EPUB 2012 MAR 17. PMID: 22424758
HEIDERSCHEIT BC, CHUMANOV ES, MICHALSKI MP, WILLE CM, RYAN MB. EFFECTS OF STEP RATE MANIPULATION ON JOINT MECHANICS DURING RUNNING. MED SCI SPORTS EXERC. 2011 FEB;43(2):296-302. DOI: 10.1249/MSS.0B013E3181EBEDF4. PMID: 20581720